With cold and flu season just around the corner and COVID still a danger, we asked some of our expert doctors at K Health what they do to protect themselves from getting sick. Over and over again, their No. 1 answer surprised us.
Among the many preventative measures they take, including getting vaccinated against flu and COVID, avoiding people who seem sick (sneezing, coughing), and wearing masks indoors, there’s one thing they always do that too many people forget: wash their hands.
“I always wash my hands before eating or touching my face, assume every door handle in a public place is covered with germs, and clean my cell phone whenever I remember,” said Dr. Chesney Fowler, Medical Director at K Health and a practicing emergency room physician. “I wish I had a more creative answer for you. It’s literally just ‘wash your hands all the time.’”
Lest you scoff at the idea that washing your hands can be the key to keeping you healthy all winter, it was the first answer given to us by most of the physicians we spoke with—and everyone mentioned it.
“In the ER, a doctor can care for 40 sick patients without getting sick herself, because we all wash our hands between every patient, wipe down our cell phones, and wipe down our keyboards,” added Dr. Fowler.
In the 1840s in the Great Hospital in Vienna, Austria, there were two maternity wards, one staffed with medical students and the other with only midwives. While the medical students split their time between helping mothers give birth and studying cadavers in the morgue, the midwives only focused on births. The student clinic had a maternal mortality rate of 10%, compared with 2% for the midwives because they weren’t infecting mothers and babies with germs from the cadavers. The hospital instituted handwashing coming out of the morgue, and maternal mortality in the medical student ward dropped to 3%.
Today, handwashing is considered the best way to prevent the spread of infectious disease by the World Health Organization, and doctors have clearly internalized the message. “Wash your hands frequently,” said Dr. David Morley, Medical Director at K Health and practicing ER physician. “Wash your hands often,” said Dr. Edo Paz, Vice President of Medical at K Health and practicing cardiologist. So, why haven’t you made it something you obsess over if you want to stay healthy?
To make it easier, the U.S. Centers for Disease Control and Prevention provides a list of “key times to wash your hands”:
- Before, during, and after preparing food
- Before and after eating food
- Before and after caring for someone at home who is sick with vomiting or diarrhea
- Before and after treating a cut or wound
- After using the toilet
- After changing diapers or cleaning up a child who has used the toilet
- After blowing your nose, coughing, or sneezing
- After handling your pet, pet food or pet waste
- After touching garbage
I don’t want you to leave this article thinking that’s the only thing you can do to stay healthy. Here are the other things doctors at K Health do:
- Get vaccinated, for both flu (annually) and COVID (everyone 12 and older is now eligible for the new Omicron booster and everyone six months and older is eligible for the initial series)
- Avoid people who are sneezing and coughing
- Consider wearing a mask when indoors and in public, especially in high-risk areas
- Drink lots of water
- Take vitamin C at the first sign of sickness
- Check symptoms with K
What Doctors Do Once They Get Sick
“I treat the symptoms, and may consider getting tested for COVID or the flu to see if I’m a candidate for antiviral medication like Tamiflu,” said Dr. Fowler.
When it comes to viral infections, there’s often little that can be done but help support the body’s immune system and try not to spread it to others.
“I stay home from work and school when I’m sick,” said Dr. Fowler, adding, “If you or a family member has a virus, clean all high-touch surfaces, wash your hands regularly, and do not share food and drink.”
In addition to all of the above, Dr. Paz also recommends wearing a mask when going out in public to prevent spread of disease to others, and to treat your symptoms with over-the-counter medications.
Here’s what Dr. Fowler keeps in her medicine cabinet for cold, flu and COVID:
- Acetaminophen and Ibuprofen (Tylenol and Advil, for fever and pain)
- Dextromethorphan (Robitussin, for cough)
- Saline nasal sprays (for stuffy nose)
- Sudafed (for nasal congestion, for older kids and adults only)
- Benadryl (for allergies, nighttime)
- Claritin, Zyrtec, and Allegra (for allergies, daytime)
If these medications don’t help much, or symptoms get worse, it may be an indication of more serious disease.
“Pay attention to worsening symptoms,” Dr. Paz said. If you experience serious symptoms, it may be time to consult a physician.
The most serious symptom you should look out for with respiratory diseases is shortness of breath. It could be a sign that your health or life are at great risk, especially if you are also dizzy and confused. At that point, it might be time to go to the emergency room.
“If you’re having trouble catching your breath, see a doctor. That isn’t just a cold,” said Dr. Fowler.
Cold, Flu or COVID: Use K Health to Help Diagnose
If you’re feeling unwell and think it might be something worse than a cold, but want to learn more before leaving the comfort of home, try K Health’s free Symptom Checker.
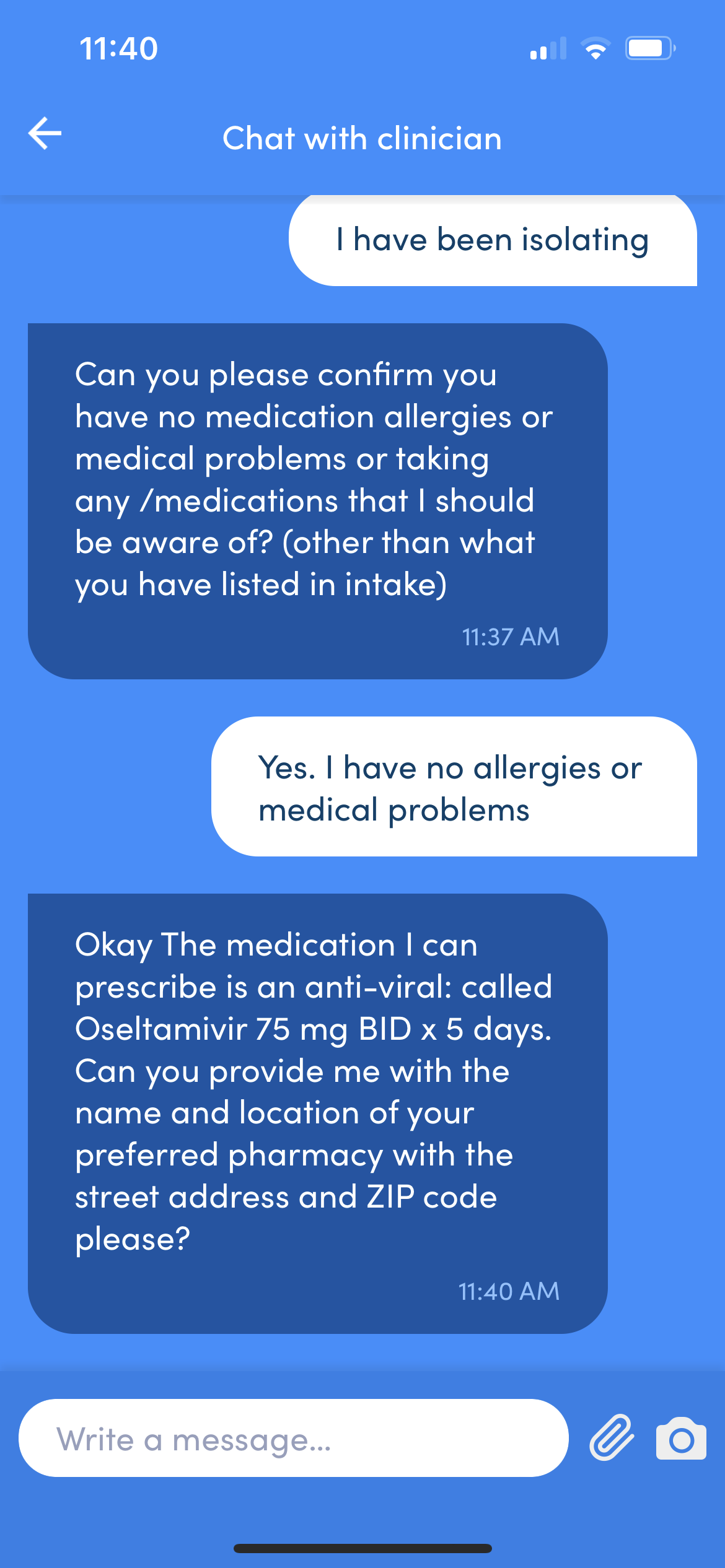
K Health’s Symptom Checker uses AI to instantly tell you how others with similar symptoms were diagnosed and treated. You enter your symptoms, and we’re able to tell you potential diagnoses, common treatments, and what to watch out for. If you want to chat with a clinician, you can connect to one instantly on our mobile or web app. Every person who uses K Health starts with the Symptom Checker so they—and their clinician—can be empowered with personalized information about their health.
A friend of mine was recently feeling sick and I thought it might be the flu. Even though it’s not exactly flu season, we are seeing some flu going around. So, I told him to use K and see what results he would get.
Turns out, more than half of people with symptoms like his had the flu, confirming what we initially thought.
When he started a visit with K Health, the clinician said that he might have the flu, but to give it a few days to see what happened with his symptoms, especially since it wasn’t during flu season. In a few days, when his symptoms worsened, he logged on again and the physician prescribed him Tamiflu, which is used to treat and prevent flu, and for someone like him, who is already experiencing symptoms, should reduce the duration of illness by 1-2 days.
FAQ
If you think you have the flu, when should you connect with a clinician?
If you cannot keep down even small amounts of liquids due to vomiting, if you haven’t urinated in 6-8 hours due to vomiting or diarrhea, if you have a stiff neck (can’t touch your chin to your chest), if you have trouble catching your breath, if you have severe abdominal pain, or if you have a weak immune system that puts you at higher risk of serious illness. If you’re caring for someone (adult or child) with the flu and they’re less arousable than normal for that time of day, they should be seen in person immediately. This is distinct from “really tired because they have a fever and want to take a nap”—do they come all the way awake or are they still out of it?
What’s worse, a persistent fever or a high fever?
A persistent fever is more worrying. Especially in kids, a child might have a really high fever like 103F. If the child is still arousable and staying hydrated, the number is not worrying. Look at the child, not at the number. If a child has a high fever, give them acetaminophen and ibuprofen, encourage hydration, and recheck it in an hour.
A fever for five days in a row merits in-person evaluation, especially in children, to check for dangerous diseases.
When you have a cold, is there any reason to see a doctor? What are the most severe cold symptoms?
If you’re having trouble catching your breath, see a doctor. That isn’t just a cold. (If you’re having severe symptoms, it’s not a cold.) If your symptoms are mild, there’s nothing that can be done to accelerate the recovery process. (Suck it up, buttercup!)
When you test positive for COVID, at what point should you consult a doctor? At what point should you seek emergency care?
Consult a medical provider virtually whenever you have questions about treating your symptoms at home, what over-the-counter medicines can be safely taken together, and what steps you should take to keep your family healthy.
Be seen in-person if your oxygen level is low (as determined by your medical provider), if you’re having trouble catching your breath (even if your oxygen level is normal), if you have an underlying medical condition that weakens your immune system (you might need antivirals or monoclonal antibodies), if you haven’t urinated in many hours and are struggling to stay hydrated, if you have significant chest pain, or any other symptoms that really worry you.
If you’re caring for someone with COVID, call 911 if they’re difficult to arouse or less alert than normal, if their skin is taking on a bluish or discolored tint, if they cannot carry on a conversation because they’re struggling to breathe, or if they have any other symptoms that make you concerned about a life-threatening emergency.
What is the most worrying early COVID symptom?
Shortness of breath. At that point, it’s time to go to the emergency room.
This article was medically reviewed by Craig Sorkin, DNP, APN.
K Health articles are all written and reviewed by MDs, PhDs, NPs, or PharmDs and are for informational purposes only. This information does not constitute and should not be relied on for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment.

 Medically reviewed
Medically reviewed